WASHINGTON — QUESTION:
Who does the CDC consider ‘health care personnel?’
Who will be among the first group to receive the COVID-19 vaccine?
ANSWER:
As defined by the CDC, health care personnel “refers to all paid and unpaid persons serving in health care settings who have the potential for direct or indirect exposure to patients or infectious materials."
SOURCES:
The Advisory Committee on Immunization Practices- Interim Recommendation for Allocating Initial Supplies of COVID-19 Vaccine — United States, 2020, slides from ACIP meetings (1, 2)
The Centers for Disease Control and Prevention- Infection Control Appendix 2 Terminology, CDC Statement Regarding ACIP Recommendations
PROCESS:
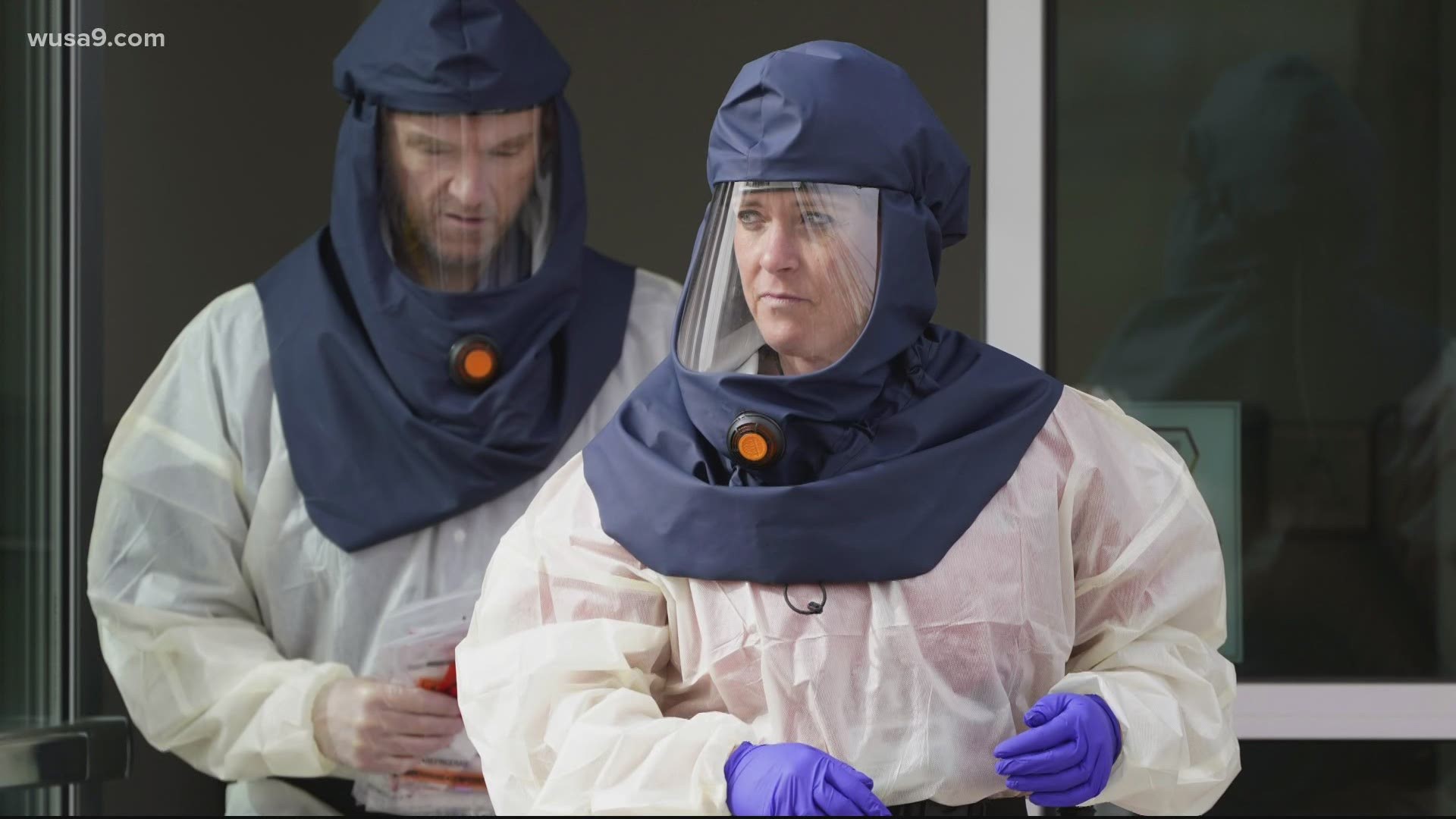
Health care workers are among the many heroes in the long battle against COVID-19. They continue to put their own wellbeing on the line to serve others, despite early months of PPE shortages and supply frustrations, treating patients with respect and compassion.
They will also be among the first on tap to get the COVID-19 vaccine when one becomes available, thanks to input from a CDC committee of doctors and scientists.
The CDC has a federal advisory committee called The Advisory Committee on Immunization Practices (ACIP), which helps make recommendations on the distribution of vaccines to the public.
On Dec.1, they recommended that healthcare personnel and those living in long-term care facilities be the first to receive the vaccine.
“As of December 1, 2020, approximately 245,000 COVID-19 cases and 858 COVID-19-associated deaths had been reported among U.S. health care personnel,” the ACIP said in their recommendation. “Early protection of health care personnel is critical to preserve capacity to care for patients with COVID-19 or other illnesses.”
On Dec. 3, CDC Director Robert Redfield formally accepted the interim recommendation.
So, who are "health care personnel” according to the CDC and ACIP?
In the ACIP’s recommendation, they point to a definition from the CDC: “health care personnel are defined as paid and unpaid persons serving in health care settings who have the potential for direct or indirect exposure to patients or infectious materials.”
ACIP breaks that down further in slideshow presentations from their meetings on Nov. 23 and Dec. 1, and in their Dec. 3 recommendation, approximating 21 million people who work in hospitals, long-term care facilities, outpatient clinics, home health care, public health clinical services, emergency medical services and pharmacies.
“Health care personnel comprise clinical staff members, including nursing or medical assistants and support staff members (e.g., those who work in food, environmental, and administrative services) (8),” the recommendation says. “Jurisdictions might consider first offering vaccine to health care personnel whose duties require proximity (within 6 feet) to other persons. If vaccine supply remains constrained, additional factors might be considered for subprioritization.*** Public health authorities and health care systems should work together to ensure COVID-19 vaccine access to health care personnel who are not affiliated with hospitals.”
It's important to remember that these are recommendations, not rules. The actual rollout could be different in different states.