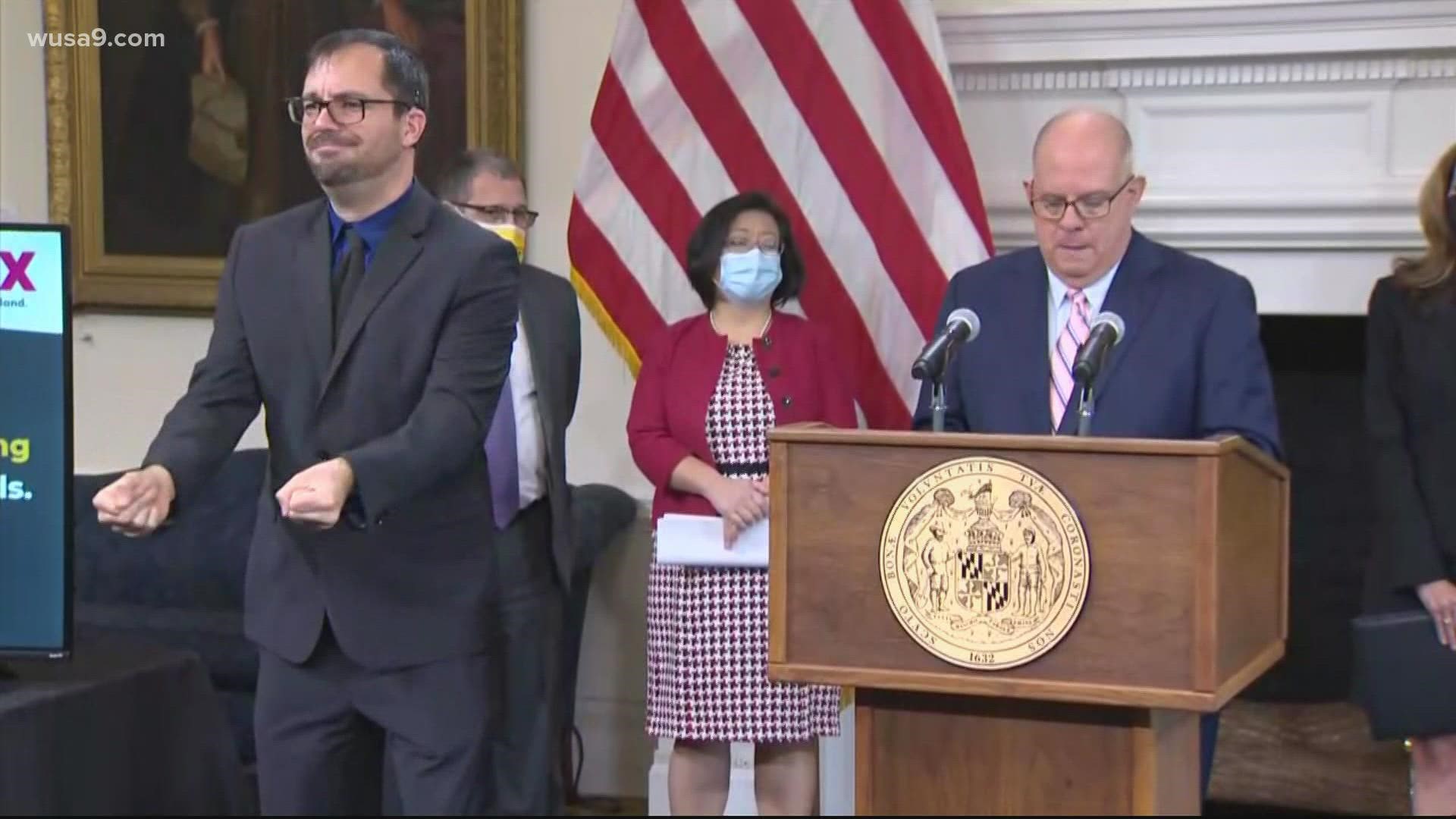
MARYLAND, USA — As Maryland COVID-19 hospitalizations approach the highest levels since mass vaccine distribution began, Gov. Larry Hogan announced a requirement for all nursing homes to offer monoclonal antibodies – even to residents who haven’t tested positive yet for the virus.
The directive issued Thursday states if a Maryland nursing home has a covid outbreak, residents who’ve tested positive, and those who still test negative, will be offered an approved or emergency authorized therapeutic treatment for covid.
The most prominent of the therapies remains monoclonal antibodies, copies of virus antibodies produced in a lab and typically injected intravenously. The treatment reduces severity of covid symptoms, along with the risk of hospitalization and death.
“These therapies (such as monoclonal antibodies) shall be offered to those residents that test positive and also as a prophylaxis for residents,” the order states.
In August, the Food and Drug Administration authorized monoclonal antibodies administered prophylactically – a precautionary measure for patients who’ve been exposed to the virus, but still test negative.
Thursday’s announcement comes as Maryland reached 1,167 covid hospitalizations, just 33 cases away from a critical benchmark. When the state reaches 1,200 virus patients in acute and ICU beds, hospitals will be required to make all staffed bed capacity available.
At that point, state health directives will also cut all non-urgent hospital surgeries with overnight stays.
At 1,500 hospitalizations, pandemic surge plans are triggered state-wide.
“Marylanders should be reassured by this order of Governor Hogan,” said Joseph DeMattos, Jr., president and CEO of the Health Facilities Association of Maryland (HFAM).
“They should be reassured in the therapy, and they should be reassured that Maryland’s skilled nursing and rehab centers have been partnering for months with the Maryland Department of Health on this front.”
DeMattos said HFAM’s 150 centers have lobbied for monoclonal antibodies to be offered in their facilities as widely as possible. But among the most frustrating hurdles still present during the current phase of the pandemic – family members tasked with medical decisions, declining recommended treatments for their loved ones.
“Oftentimes, the medical decision maker, is different from the patient or the resident,” DeMattos said. “And that’s an added hurdle with getting any drug or any therapy into the arm of a patient.”