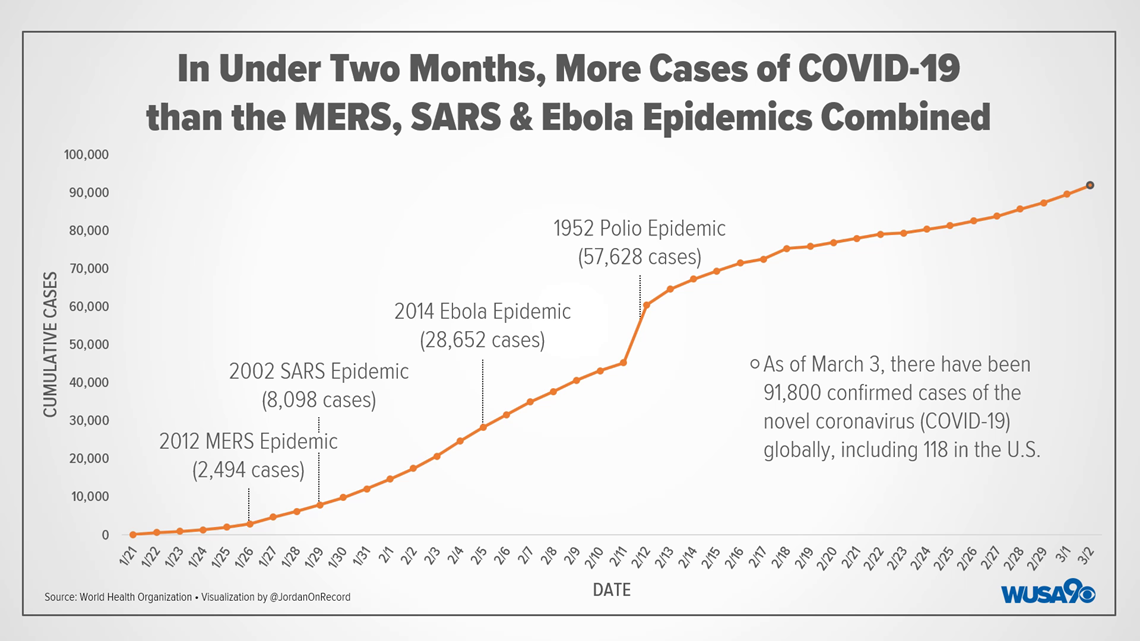
WASHINGTON — While there are still no confirmed cases of the novel coronavirus, or COVID-19, in the D.C. metro area, worldwide, the virus has already become one of the most prolific epidemics in recent memory
As of March 3, the World Health Organization reported more than 91,800 confirmed cases of the coronavirus worldwide. While most of those cases have been in mainland China – approximately 80,270 of them, cases have been identified in more than 80 countries worldwide. In the U.S., at least 118 people have been confirmed to have the virus so far.
Those numbers mean that, in the less than two months world health authorities have been tracking the virus, COVID-19 has already spread to more people than the 2002 SARS, 2012 MERS and 2014 ebola epidemics. The virus has now spread to more people than the worst year of the peak of the polio epidemic in the U.S.

Scientists describe how infectious a disease is using a measure called a reproductive number, or R0 (pronounced R-naught). It is, roughly, the estimated number of people who will catch the disease from a single contagious person. The common flu, for example, has an R0 of about 1.3. One of the most infectious diseases is the measles, which has an R0 ranging from 12-18.
Estimates for COVID-19’s R0 range from as low as 1.4 to as high as 6.5 – a range covering the H1N1 swine flu at the low end and the highly contagious small pox on the high end. Which is to say: Epidemiologists just aren't sure yet.
But, the R0 alone can’t tell you everything about how easily a disease will spread. The flu, for example, has a relatively low R0, and yet millions of people are infected with it each year in the U.S. Measles on the other hand is extremely contagious, and yet less than 1,300 cases were reported in the U.S. last year.
This is explained by a few things, not the least of which is the presence and widespread adoption of a vaccine for the measles. While vaccines for the flu are available, they typically only cover a portion of the most common strains, and, because of the huge numbers of infected persons, the flu is constantly mutating.
Where COVID-19 has proven to be less serious than recent epidemics so far has been in its mortality rate. Although it has been transmitted to a far larger number of people than the 2002 SARS or 2012 MERS epidemics (both SARS and MERS are variants of the coronavirus, incidentally, and prior to its classification as COVID-19, the current coronavirus’ name was SARS-CoV-2), a much smaller portion of those cases have resulted in deaths.
Of the 93,158 COVID-19 cases confirmed so far worldwide, only 3,198 have resulted in death – a mortality rate of 3.4%. By comparison, the 2002 SARS outbreak had a mortality rate of 10%, and, despite having fewer than 1,000 cases worldwide, the 2003 Avian Flu (H5N1) outbreak caused 455 deaths – a mortality rate of 52.8%. For further comparison, the current U.S flu season – which has topped 30 million confirmed cases so far – has a mortality rate of around .1%. Before it was eradicated, small pox had a mortality rate of 30% or higher.
Despite all of that, because of its high transmission rate, COVID-19 has now resulted in more total fatalities than the MERS, SARS and ebola epidemics combined.
While the number of U.S. cases has remained small so far, that count is likely to rise in the near future as the CDC expedites nationwide distribution of the tests needed to identify COVID-19. And on Tuesday, Vice President Mike Pence, who is leading the White House’s coronavirus taskforce, said new guidance was being issued to allow anyone to get tested for the virus.
"Several governors said to me that there was an impression that the test would not be administered to people who were only mildly symptomatic,” Pence said during a briefing. “We are issuing new guidance, effective immediately, from the CDC that will make it clear that any clinician on health authority can administer the test."
To date, only nine patients have been confirmed to have died from COVID-19 in the U.S. All of them were located in the state of Washington.