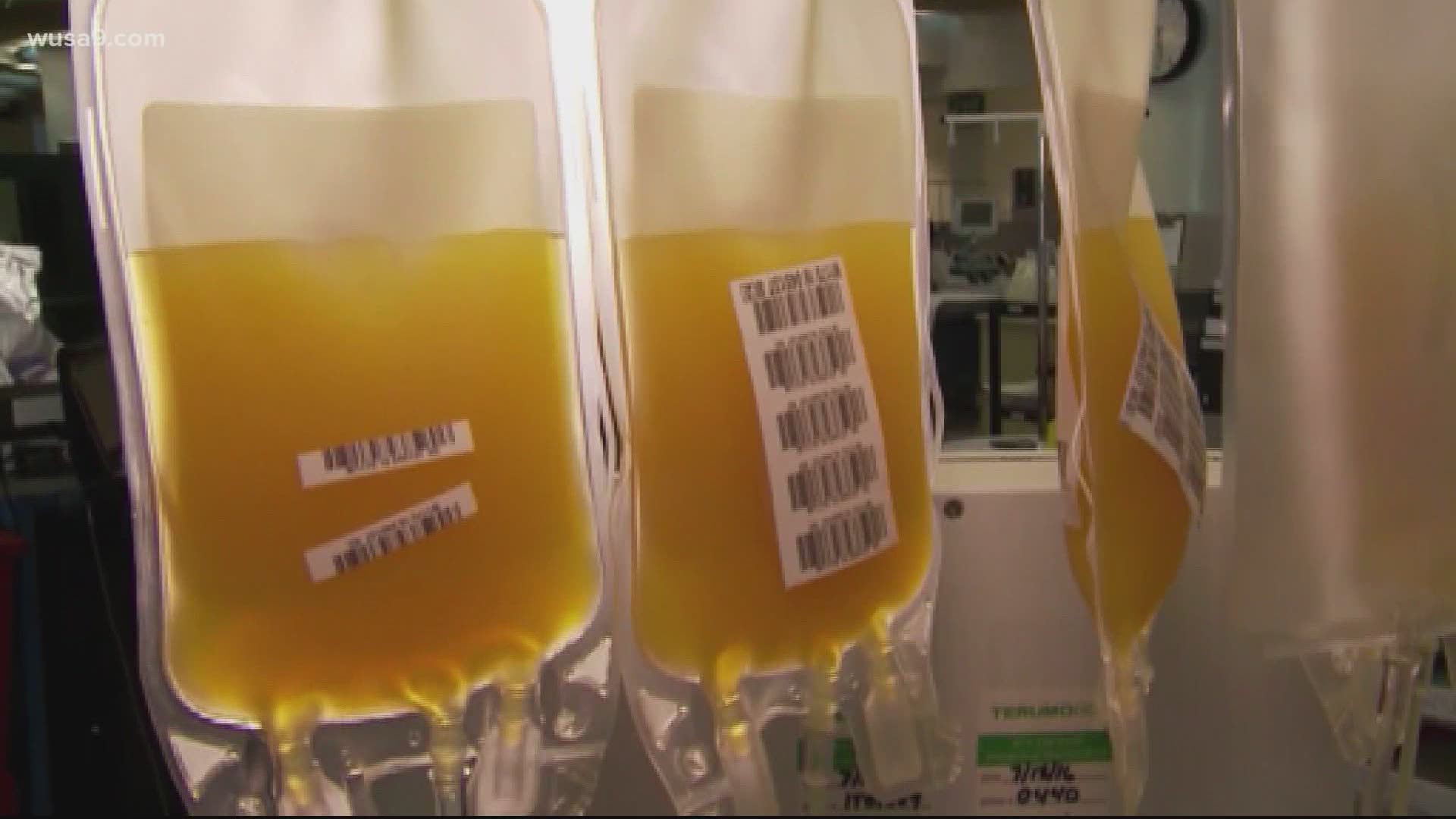
WASHINGTON — Over the last few days, there have been a lot of questions about the efficacy of convalescent plasma as a treatment for COVID-19. The FDA-approved Emergency Use Authorization of it for the treatment of hospitalized patients. But many top doctors say that decision was made too hastily.
Still, studies of convalescent plasma continue and scientists are looking into how its use could potentially impact people before they end up in the hospital.
Johns Hopkins University is working on two clinical trials using convalescent plasma. The QandA team spoke to a few of the doctors participating in the studies who said the out-patient treatments they’re working on could provide temporary immunity to bus drivers, metro workers, teachers and others who are at high risk of exposure to the virus.
But first, we asked them what they thought about the FDA’s decision.
Ariane: What is your opinion of the FDA’s decision to approve convalescent plasma as a treatment for COVID-19 patients and how does that impact your studies?
Dr. David Sullivan: They made the decision that they were unlikely to gather more information that would be helpful to the decision, and that the benefit was significant. I don't have a quarrel with that decision.
Dr. Daniel Hanley: We're not quarreling with the decision that it works in hospitalized patients, but we want to try it and see if it works better earlier by focusing on the outpatients.

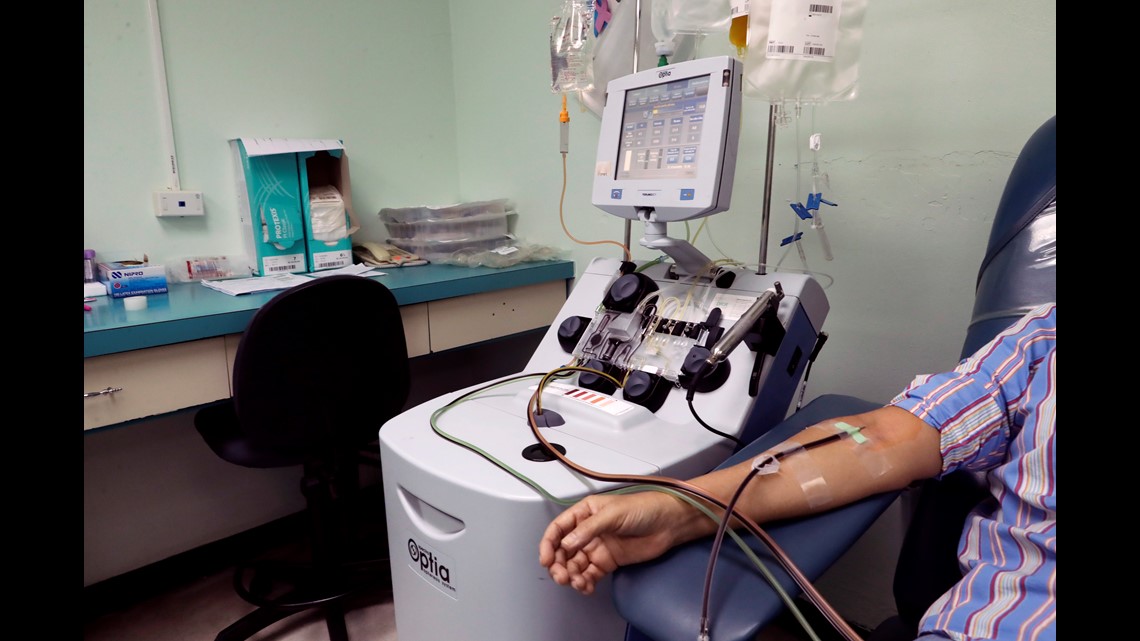
Doctors Daniel Hanley and David Sullivan are two of the many doctors working on two studies of convalescent plasma as a treatment for COVID-19 at Johns Hopkins University. Through their out-patient research, the scientists hope to do two things: prevent people infected with COVID-19 from having to go to the hospital and prevent the conversion of exposure to the virus to infection.
Ariane: What makes your trials different from the ones used to support the FDA’s decision to approve Emergency Use Authorization convalescent plasma for the treatment of COVID-19?
Dr. David Sullivan: This is the highest level of evidence and the most important kind to gather: it’s a randomized control blinded study.
Ariane: Do you anticipate that your findings will replace the need for a vaccine?
Dr. Daniel Hanley: Instead of waiting on a vaccine to generate antibodies over a month, we are taking pre-existing antibodies from people that are recovered and immediately giving him to recipients who are newly diagnosed with COVID-19, or have a high-risk exposure.
Ariane: So it's not a replacement for a vaccine it's in intermediate until we get there.
Dr. Daniel Hanley: Right. People that are really at high risk of acquiring the disease but get treated about once every two months -- avoid the consequences of the disease, or infection. That's the idea. It's called passive immunization. But even when we have a vaccine, not everyone is going to get a vaccine and even those who do, not everyone will respond to a vaccine. So convalescent plasma is still a method of developing immediate immunity, immediate antibodies that mimics a vaccine.
Ariane: So if this treatment works, how often will people need to get it?
According to Dr. Hanley, the trial that’s studying whether the convalescent plasma can stop people that are at high risk of exposure from contracting the virus would require patients to receive the outpatient treatment once every one to two months.
The doctors say these two clinical trials have only studied about 10% of the patients needed in order to get conclusive evidence to support or refute their theories. There are 4 locations in the DMV where the trial is taking place. To find out if you qualify to participate in the study. Go to covidplasmatrial.com